Finding Your People: Building a Grief Support System That Actually Helps
Discover how to build a grief support system that truly helps. Learn how to identify your inner circle, find compassionate companions, and create a network that supports healing on your terms.

Key Takeaways
- Grief support isn't about "getting over it" but about having people who understand while you integrate loss into your life
- Your support needs will change over time, and different people in your life can help with different aspects of grief
- Asking for specific help (rather than general support) makes it easier for others to show up meaningfully
- Professional grief support and community connections serve different but equally important roles
- Building a support system isn't about replacing your loved one, it's about creating space to honor them while you heal
Reflections on love, loss, and the many ways we carry them.
If you’re reading this and feeling painfully alone in your grief, I want you to know that you are not alone. That hollow distance you feel, even when surrounded by people, is something I hear from grieving clients all the time. Loss alters the way we connect. It rearranges the emotional furniture inside us, making familiar relationships suddenly feel foreign. And yet, what you’re experiencing makes perfect sense. Our brains are wired to heal through connection. When we grieve in isolation, we’re working against our own biology.
One client, whom I’ll call Mina, once told me, “Cathy, I didn’t know how to ask for help. I didn’t want to bother anyone. Then one morning, I realized I hadn’t spoken to a single person about my husband in weeks.” Her sadness wasn’t just from grief, it was from carrying it alone. When we explored the science together—that grief activates the brain’s physical-pain pathways, that cognitive fog is normal, that support is not indulgence but medicine, her shoulders dropped in relief. “So I’m not failing?” she asked. Not at all. She was human.
Research shows that healthy grieving isn’t about “moving on” but integrating the loss through continuing bonds, ongoing connection, meaning-making in your own time. And connection doesn’t come from crowds; it comes from a few people who can sit with your truth without turning away.
Parting Stone’s work reminds us that grief doesn’t need correcting. It needs companionship. So reach out. Ask for help. Let yourself be held. Healing, after all, is a shared act.
Cathy Sanchez Babao
Parting Stone Grief Coach
The Weight of Grieving Alone
If you're reading this feeling isolated in your grief, you're not imagining it. The loneliness that accompanies loss can be profound, even when you're surrounded by people. What you're experiencing makes sense. Grief changes how we connect with others, and many people find themselves pulling back or feeling misunderstood precisely when they most need support.
Here's something important to know: needing help with grief isn't a sign of weakness or dysfunction. Research consistently shows that social support is one of the most significant predictors of healthy grief adaptation (Stroebe & Schut, 1999). Your brain and body are wired to process difficult experiences through connection with others. When you grieve alone, you're working against your natural healing mechanisms.
The difficulty isn't just in feeling alone. It's in knowing you need support but not knowing how to ask for it, who to turn to, or even what kind of help would actually be useful. Many grievers describe feeling like a burden, worrying they've already talked about their loss too much, or sensing that others are uncomfortable with their ongoing sadness.
David from New York 🖤 shares, "When my brother passed away unexpectedly, our family was devastated. I keep one in my pocket and touch it throughout the day. It helps me feel like my brother is still with me." His experience reflects a common truth: connection to our loved ones and connection to our support network often work together in the healing process.

A New Way to Hold Close What Matters Most
We transform cremated remains into beautiful, touchable stones that bring comfort when you need it. Something you can hold, share, and keep close.
Understanding Why Grief Support Matters
Your brain under grief isn't functioning the way it normally does. Neuroscience research shows that grief activates the same neural pathways involved in physical pain (O'Connor et al., 2008). This isn't metaphorical. The ache you feel is being processed by pain centers in your brain. Just as you wouldn't expect to recover from a serious injury alone, grief requires outside support for healthy healing.
Grief also affects your prefrontal cortex, the part of your brain responsible for decision-making, planning, and emotional regulation. This is why many grievers describe "grief brain": difficulty concentrating, making decisions, or remembering things. When your cognitive resources are depleted by loss, having a support system provides external structure and helps carry some of the mental and emotional load.
But support isn't just about managing symptoms or getting through each day. Research on continuing bonds theory has shown that healthy grief isn't about severing connection to the deceased; it's about finding new ways to maintain relationship with them while building a life that integrates their absence (Klass et al., 1996). Support helps you do this work. Other people can hold memories with you, help you make meaning from loss, and witness your transformation as you figure out who you are now.
The goal isn't to "move on" or reach some mythical state of "closure." Those concepts don't reflect how grief actually works. The goal is integration: learning to carry your loss while still engaging with life, relationships, and eventually, joy. Support systems make integration possible by providing scaffolding during reconstruction.
@chloebluffcakes Thank you @partingstone 🤍 youve given me an unimaginable gift. One day I will share these with my little sister and carry her wherever we go in life together. #grief #partingstone #loss
♬ Repeat Until Death - Novo Amor
What Kind of Support Do You Need When Grieving?
Grief support isn't one-size-fits-all. What helps one person might feel wrong for another, and what you need today will likely differ from what you need six months from now. Understanding the different types of support can help you identify what's missing and where to look for it.
Emotional support involves people who can listen without fixing, validate your feelings without minimizing them, and sit with you in discomfort without rushing you toward positivity. These are the people who say "This is really hard" instead of "Everything happens for a reason." Emotional support doesn't solve problems; it witnesses them.
Practical support addresses the concrete tasks that become overwhelming during grief. This might include help with meals, childcare, household maintenance, or managing the logistical aftermath of loss (paperwork, estate matters, memorial planning). Practical support is often easier for people to provide and for grievers to accept because it feels less emotionally vulnerable.
Informational support comes from people who can help you understand what you're experiencing or navigate unfamiliar territory. This might include guidance from others who've experienced similar losses, information from grief counselors about normal grief responses, or recommendations about memorial options and end-of-life decisions.
Memorial and commemorative support involves people who help you honor your loved one's memory in ways that feel meaningful. This could be family members participating in remembrance rituals, friends sharing stories and memories, or professionals who understand the importance of physical connections to the deceased.
Karen in Wisconsin 🖤 describes how different types of support converged: "This made sharing with family and special friends easy. I look at the stones I keep on my coffee table in a way not possible with an urn, and feel great respect, connection, and comfort." Her experience illustrates how memorial decisions become easier when your support system helps you explore options that feel right for your unique grief.
Your support needs will shift as grief evolves. Early grief often requires more practical and emotional support. As time passes, you might need more informational support (understanding grief waves, anniversary reactions) or commemorative support (creating ongoing rituals, making memorial decisions when you're ready).
Cremated remains can feel messy and meaningless. Instead of receiving a box of ashes following cremation, you can now receive a collection of stones. Solidified remains let you feel connection with the remains of your departed. Turn your ashes into stones at https://partingstone.com
Building Your Personal Grief Support System
Think of your grief support system as concentric circles radiating outward from you. Each circle represents a different level of intimacy and type of support. Building this system isn't about having dozens of people; it's about identifying a few key individuals in each circle who can help in specific ways.
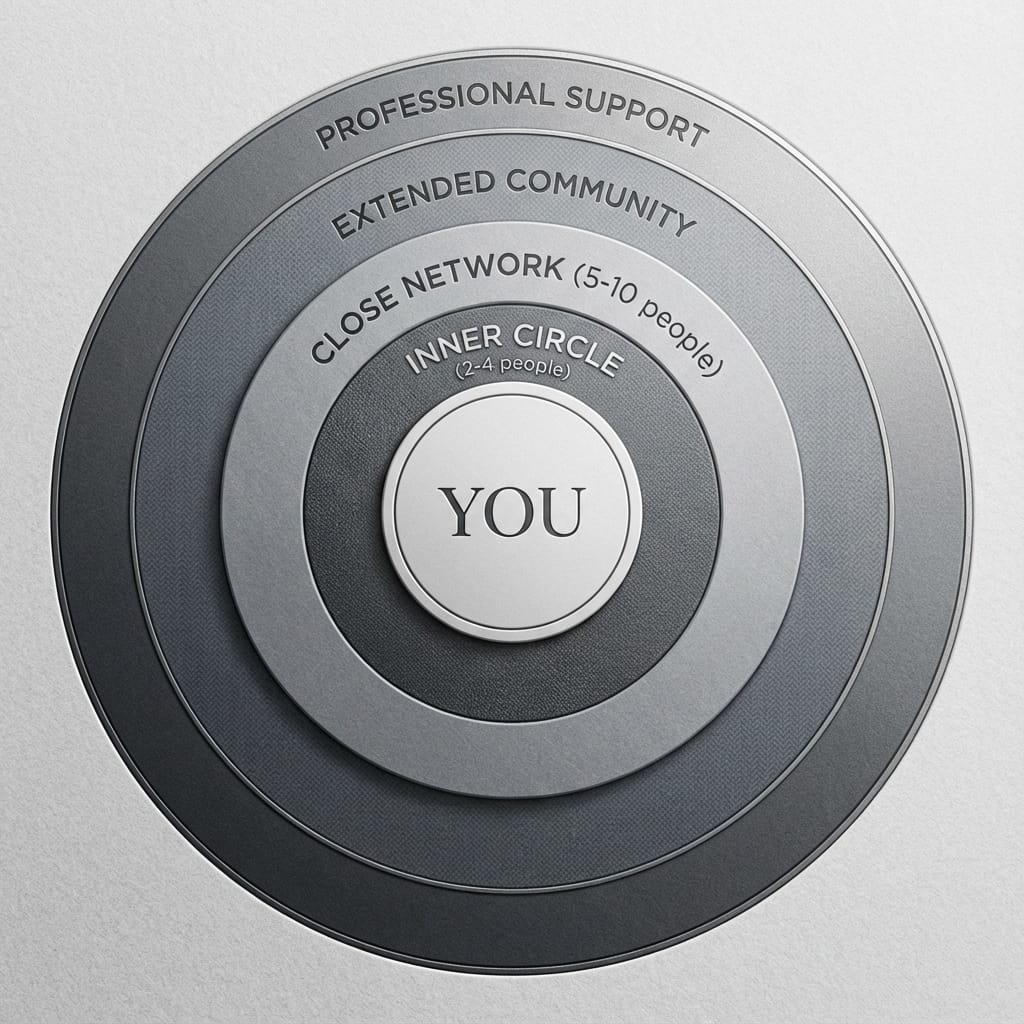
Your Inner Circle
These are 2-4 people who can handle the rawness of early grief, who you can call at 2am, who won't judge your worst moments. They might be a spouse, sibling, best friend, or parent. The key characteristic is their ability to be present without needing you to perform okayness.
Identifying your inner circle requires honesty about who has actually shown up, not who you wish would show up. Some people we expect to be there aren't, and that's a secondary loss that deserves acknowledgment. Meanwhile, sometimes people surprise us with their capacity for presence.
MaryJayne from Albuquerque, New Mexico 🖤 shares, "I think having the stones rather than just ashes or a burial is that the stones are beautiful, they can be shared with loved ones and can be placed in sites that are meaningful to the family or that were meaningful to the deceased." Her words reflect how inner circle support often involves shared decision-making and collective remembrance.
Your Close Network
This circle includes 5-10 people who provide specific types of support. One friend might be great at practical help but uncomfortable with emotional conversations. A sibling might excel at remembering your loved one but struggle with checking in regularly. A coworker might offer excellent advice about grief and work boundaries.
The key is matching people to their strengths rather than expecting everyone to provide all types of support. This also protects you from disappointment and helps others feel more confident in their role.
Extended Community
This circle includes grief support groups, online communities, faith communities, or social connections that provide ambient support. You might not share your deepest struggles here, but these connections combat isolation and provide normalizing experiences. Seeing others who are months or years ahead in their grief journey can offer hope that integration is possible.
Professional Support Layer
This includes grief counselors, therapists, support group facilitators, or other professionals who provide structured guidance. Professional support isn't a sign that your personal network has failed; it's a specialized resource that addresses aspects of grief your friends and family can't.
Try This: Create a support inventory. Draw the concentric circles and write names in each one. Then note what type of support each person provides. Look for gaps. Do you have emotional support but no practical help? Lots of people who care but no one who really understands your specific loss? This isn't about judging what you have; it's about identifying what's missing so you know where to focus your energy.

How to Ask for the Help You Actually Need
Asking for help might be the hardest part of building a grief support system. Many grievers describe feeling like they're burdening others, that they've already talked about their loss too much, or that people are tired of hearing about it. These feelings are common, but they're often not accurate reflections of others' willingness to help.
The discomfort of asking is normal. Grief makes us vulnerable, and vulnerability with other people requires trust and courage. But here's what research shows: people generally want to help, they just don't know how (Breen & O'Connor, 2011). When you give specific directions, you make it easier for them to show up in ways that actually matter.
Be Specific Rather Than General
"I need support" is overwhelming and unclear. "Could you come over Thursday afternoon and sit with me while I sort through some of mom's things?" is actionable. Specific requests work better because they reduce the guessing game and let people know exactly what would help.
Sample Scripts for Different Situations:
- To a close friend: "I'm having a really hard week and I need to talk about [name]. Could we get coffee Saturday morning? I just need someone to listen, not necessarily fix anything."
- To a family member: "I'm not ready to make decisions about the memorial yet, but I will be soon. Would you be willing to help me research options when I'm ready? Maybe in a few weeks?"
- To a colleague: "I'm back at work but I'm still grieving. Some days are harder than others. If I seem off, it's not personal. I might need occasional flexibility with deadlines."
- To your partner: "I need you to check in with me about how I'm doing, not just assume I'm okay. Even if I say I'm fine, could you ask what I'm really feeling?"

Different Approaches for Different Relationships
How you ask for support depends on the relationship and the person's comfort level with grief. Some people excel at practical help but freeze with emotional needs. Others are natural emotional supporters but terrible at follow-through on tasks.
For action-oriented people, give them a job: "Could you organize a meal train?" or "Would you handle the thank-you notes for flowers?" For emotionally attuned people, be direct about emotional needs: "I need someone to just listen without trying to cheer me up."
Alli from Colorado 🖤 explains how her family created collective support: "Parting Stone allowed all of our family members to have a couple of stones to serve as mementos. My mom loved to travel so we take the stones with us each time we travel and share our adventures in photos through a group chat. It's a fun way to keep in touch and remember our mom." This illustrates how support can be both practical and emotionally connecting.
When Requests Aren't Met with Understanding
Not everyone will respond well, and that hurts. Some people are uncomfortable with grief. Others have their own unprocessed losses that make your grief triggering. Some simply don't have the capacity right now.
When someone can't or won't provide support, it doesn't mean your needs are unreasonable. It means that person isn't able to be in that role right now. This might mean adjusting your expectations, finding support elsewhere, or in some cases, letting relationships naturally drift if they're consistently unhelpful or harmful.
You're allowed to feel disappointed, angry, or hurt when people don't show up. Those are secondary losses that deserve acknowledgment. But dwelling on who isn't there can keep you from fully receiving support from those who are.
Try This: Practice asking for micro-help. Start with small, specific requests that feel less vulnerable. "Could you text me tomorrow to see how I'm doing?" is easier than "Will you be my grief support person?" Small successful asks build confidence for bigger requests.

Types of Professional Grief Support
Professional support serves a different function than support from friends and family. Friends provide love and connection; professionals provide structure, expertise, and objective guidance. You might need both, or you might find that personal support is sufficient. There's no "should" here.
Grief Counselors vs. Therapists
Grief counselors typically focus specifically on bereavement and helping people navigate the practical and emotional challenges of loss. They might offer time-limited support (8-12 sessions) focused on grief adjustment. Many funeral homes and hospices offer free or low-cost grief counseling.
Therapists, particularly those specializing in grief and trauma, can address more complex grief reactions or situations where grief has triggered or intensified mental health concerns (depression, anxiety, PTSD). Therapy tends to be longer-term and addresses how grief intersects with other life challenges.
Some people benefit from both: short-term grief counseling after the loss, then longer-term therapy to process complicated family dynamics, trauma, or mental health impacts.

Finding Qualified Professionals
Not all therapists are trained in grief work, and not all grief counselors are a good fit for every griever. Look for credentials like certification from the Association for Death Education and Counseling (ADEC) or specialized training in grief therapy models like Complicated Grief Treatment or Meaning Reconstruction.
The National Alliance for Grieving Children, the Dougy Center, and Psychology Today's therapist finder can help locate grief-informed professionals in your area. Many now offer telehealth, which expands options for people in rural areas or those who prefer remote support.
Questions to Ask Potential Counselors or Therapists:
- What training do you have in grief and bereavement?
- What's your approach to grief? (Listen for responses that honor individual timelines rather than stage-based expectations)
- How do you handle clients who aren't "getting better" on a particular timeline?
- What's your experience with [specific type of loss: suicide, child death, traumatic loss, etc.]?
Cost Considerations
Professional support costs vary widely. Some options include:
- Hospice bereavement programs (often free for 13 months after death, regardless of whether hospice services were used)
- Employer assistance programs (EAPs) typically cover 3-8 free sessions
- Sliding scale therapists adjust fees based on income
- Online therapy platforms sometimes cost less than traditional in-person care
- Support groups (usually free or low-cost)
Many therapists bill insurance for grief counseling under mental health coverage, though coverage varies. Don't let cost assumptions prevent you from exploring options. Many communities have free or low-cost resources specifically for bereaved individuals.
When Professional Support Becomes Essential
Some grief reactions benefit significantly from professional intervention. These include:
- Thoughts of harming yourself or persistent wish to die
- Inability to function in daily life months after loss
- Substance use to cope with grief
- Complicated grief reactions (intense preoccupation with the deceased, difficulty accepting the death, feeling life is meaningless without them)
- Trauma symptoms related to how death occurred
- Grief compounded by existing mental health conditions
Professional support at these times isn't optional; it's healthcare. There's no virtue in suffering alone when evidence-based treatments exist.
Anne in Virginia 🖤 notes, "I keep a stone in the car; I love this when I travel to a beloved location and I talk to Jack." Her words illustrate how professional support and personal coping strategies work together. A grief counselor might help you develop rituals like this that maintain connection while supporting integration.

Grief Support Groups and Communities
Support groups provide something unique: connection with people who genuinely understand because they're walking a similar path. Unlike well-meaning friends who haven't experienced your type of loss, group members "get it" without lengthy explanations.
Types of Groups Available
Diagnosis-specific groups serve people who've lost someone to particular illnesses (cancer, Alzheimer's, addiction, suicide). Shared understanding of disease progression, medical decisions, and specific grief challenges creates immediate connection.
Relationship-specific groups gather people who've lost the same relationship type (widows/widowers, bereaved parents, siblings, children who've lost parents). Relationship-specific groups address unique challenges (parenting while grieving, identity loss after spousal death, sibling grief invisibility).
General bereavement groups welcome anyone grieving any type of loss. The diversity of experiences can be valuable, though some people prefer the specificity of diagnosis or relationship-based groups.
Online communities include forums, Facebook groups, Instagram grief accounts, and platforms like Reddit's grief communities. Online support works well for people with scheduling challenges, social anxiety, or those who prefer written processing over face-to-face interaction.
How to Evaluate If a Group Is Right for You
Not every group will fit. Some are too structured; others too open-ended. Some focus heavily on religious or spiritual frameworks; others are secular. Some encourage emotional expression; others emphasize practical coping strategies.
You're looking for a group where:
- The facilitation style feels supportive, not directive
- You see yourself reflected in at least some other members
- The overall tone balances honesty about pain with hope for integration
- Ground rules create safety (confidentiality, no advice-giving, respect for different grief expressions)
- You feel slightly uncomfortable in a growing-edge way, not traumatized or retraumatized
Try This: Attend 2-3 sessions before deciding if a group fits. First sessions often feel awkward regardless of group quality. If after three sessions you still feel out of place, it's okay to try a different group or decide group support isn't for you right now.
Building Connections Without Pressure
Support groups work best when you approach them as places to give and receive, not just to take. Witnessing others' grief and offering validation can be part of your own healing. But there's no requirement to befriend everyone or become deeply involved. Some people find immense value in groups while maintaining boundaries about outside-group connection.
You're allowed to join and leave groups as your needs change. Many people participate actively in early grief, then gradually taper participation as they build other support systems. Some return for anniversary reactions or new grief waves. Healthy groups normalize this natural ebb and flow.
Elizabeth from Norwalk, Connecticut 🖤 shares, "Being able to hold my mom close and place her in her favorite spots has been incredibly powerful. Our entire family and close friends have a piece of her and it means the world to us." Her experience shows how support systems and memorial decisions often intersect, with different people in your network helping you honor your loved one in varied ways.

When Your Current Support System Isn't Working
Sometimes despite your best efforts, your existing support system isn't meeting your needs. This doesn't mean you've failed or that you're too needy. It means circumstances, people's capacity, or the match between what you need and what others can offer isn't working right now.
Signs You Need Different or Additional Support
You might need to adjust your support system if:
- You consistently feel worse after interactions with certain people
- Your supporters seem burned out or frustrated with your grief timeline
- You're protecting others from your real feelings
- Conversations feel performative rather than genuine
- No one in your life shares the specific type of loss you're experiencing
- Your needs have changed but your support system hasn't adapted
These aren't criticisms of you or your people. Sometimes mismatches happen. Recognizing them is the first step toward building what actually works.
How to Add New Support Without "Replacing" Existing People
Adding new support sources doesn't mean abandoning relationships that have been there from the beginning. Different people serve different functions. Your sister might be perfect for remembering your loved one but terrible at checking in regularly. A grief support group member might provide understanding your sister can't, but your sister knows your whole history in ways group members never will.
Frame additions as expansion rather than replacement: "I'm joining a bereaved parents group because I need to connect with others who understand this specific loss. It doesn't mean you haven't been helpful; it means I need something additional that none of us expected I'd need."
Addressing Toxic Positivity or Unhelpful Responses
Some support attempts harm more than help. Toxic positivity (forced cheerfulness, minimizing pain, rushing toward silver linings) invalidates grief rather than supporting it. Unhelpful responses include comparing grief, offering religious platitudes to nonreligious grievers, or implying timelines for "being over it."
You're allowed to set boundaries with unhelpful support, even when people mean well. Scripts for this include:
- "I know you're trying to help, but when you say [specific phrase], it actually makes me feel worse. What would help more is [specific alternative]."
- "I need you to understand that my grief isn't going to follow a particular timeline. I need support without questions about when I'll feel better."
- "I appreciate that you care, but I'm not looking for silver linings right now. I just need someone to acknowledge that this is really hard."
Some people will adjust their approach. Others won't or can't. For relationships where boundaries don't improve the dynamic, you might need to reduce contact or redirect those relationships away from grief topics.
Self-Advocacy Strategies
Advocating for your grief needs is a skill that develops over time. It requires:
- Clarity about what you actually need (often learned through trial and error)
- Willingness to disappoint people who want you to grieve differently
- Capacity to recognize when you're not being supported well (even by people who love you)
- Courage to make changes that serve your healing rather than others' comfort
Self-advocacy isn't selfish. It's recognizing that you're the expert in your own grief and that protecting your healing process is necessary, not optional.
Rhonda Lipinski from Elbert, Colorado 🖤 explains, "Parting Stones kept me informed of the process all along the way and that was reassuring. The final product was presented in a cherished manner and sharing them with family members who live far away has been a wonderful way to keep him in their homes and hearts." Her words illustrate how good support includes clear communication, emotional attunement, and respect for what matters to the griever.
The cremated remains of Garth's mother felt meaningless sitting in his clothing closet for 2 decades. Learn how solidified remains helped dissolve the relationship barrier he felt with her and integrate her memory into daily life.
Supporting Yourself Through Memorial Decisions
Grief involves countless decisions, and many of them feel overwhelming when you're already depleted. One category that carries particular weight is memorial decisions: what to do with cremated remains, how to honor your loved one, what rituals feel meaningful, and how to create ongoing connection.
Support systems play a crucial role in these decisions. Not because others should decide for you, but because processing options, exploring feelings, and thinking through implications is easier with trusted people alongside you.
How Support Helps with All Grief-Related Decisions
Good support doesn't tell you what to do. It helps you think through options, validates the difficulty of deciding, and provides information without pressure. When you're deep in grief, decision-making capacity is compromised. Having people who can help you evaluate choices without imposing their own preferences is invaluable.
Memorial decisions often happen on different timelines for different people. Some families need to decide quickly. Others benefit from waiting until they're emotionally ready. There's no universal right timing, and support systems help you honor your own readiness rather than external pressures.
Memorial Planning as One Decision Among Many
Memorial choices sit within a larger landscape of grief decisions: continuing or changing traditions, handling belongings, telling stories about your loved one, and how to maintain connection while building a life that integrates their absence.
When considering memorial options, you might explore traditional choices (burial, keeping cremated remains in an urn, scattering) or alternatives that offer different types of connection. One option that some families find meaningful is solidified remains, a complete alternative to traditional cremated ashes.
Solidified remains transform cremated remains into smooth, stone-like forms that can be held, shared among family members, and placed in meaningful locations. Unlike traditional ashes, which can feel difficult to interact with or divide, solidified remains offer a tangible way to maintain physical connection while allowing each family member to have something they can hold and cherish.
Sandy from Portland, Oregon 🖤 describes her experience: "I wanted something to touch and hold and see. I always carry him with me. I also have a place in my home where the stones are in a clear decorative jar and he can see what's going on. Our grandsons each have 3 stones on their bedroom dresser." Her words illustrate how memorial decisions work best when they align with your specific needs for connection and remembrance.
The process of creating solidified remains typically takes 8-10 weeks and results in 40-80+ stones that can be shared, displayed, carried, or placed in locations that held meaning for your loved one. The service is available through funeral home partners nationwide, with pricing for human remains at $2,495 and for beloved pets at $1,195.
What matters most isn't which memorial option you choose, but that your choice aligns with how you need to maintain connection. Your support system can help you explore options, talk through feelings, and decide what feels right for you and your family. Some families know immediately what they want. Others need time to discover what would be most meaningful. Both paths are valid.
Making Decisions When You're Ready
Memorial decisions don't have expiration dates. If you're not ready now, that's okay. Cremated remains can be stored safely for as long as needed until you have clarity about what feels right. Rushing a decision to satisfy others' timelines or because you think you "should" have decided by now often leads to regret.
Your support system's role is to give you permission to move at your own pace while providing information and perspective when you're ready to explore options. The best support respects that only you know when it's time to make these decisions.
@mikkzazon The company is @PartingStone ♥️ #partingstones #griefjourney #griefawareness
♬ original sound - Mik Zazon
Maintaining Your Support System Over Time
Grief support isn't just for the early months. Loss creates ongoing needs that shift and change as you move through different phases of integration. Maintaining support systems over time requires intentional effort and recognition that what helped initially might need adjustment.
Long-Term Grief Support Needs
The intensity of grief typically changes over time, but the need for support doesn't disappear. Many people describe how support dropped off after the first few months, right when they were coming out of shock and truly feeling the magnitude of loss.
Long-term support looks different from early grief support. It might involve:
- People who remember your loved one and speak their name naturally
- Friends who check in on difficult days (anniversaries, birthdays, holidays)
- Companions for milestone moments (first vacation without them, first major holiday)
- Witnesses to your transformation and growth
- Connections that allow you to be your whole self, including the parts forever changed by loss
Kenneth from Arkansas 🖤 shares, "Contrary to typical ashes retained in a container or 'lost' forever when cast 'to the winds', the Parting Stones give me a lasting genuine part of my wife that I can proudly display and gain comfort if carried." His experience, years after loss, illustrates how good memorial decisions continue providing support over time.
Anniversary Reactions and Milestone Moments
Anniversaries, birthdays, holidays, and milestone dates often trigger intensified grief responses. These reactions are normal and don't mean you're regressing or failing to heal. They're part of how humans process ongoing loss.
Support during anniversary times might look like:
- People remembering without you having to remind them
- Permission to feel however you feel (sad, angry, numb, or even okay)
- Companions for rituals or remembrance activities
- Understanding when you need to change plans or traditions
Some people need active support during difficult dates; others prefer quiet acknowledgment. Your support system works best when people ask what would help rather than assuming.
How Support Needs Evolve
Early grief often requires more intensive emotional and practical support. As time passes, support needs typically become less frequent but remain important. You might need:
- Less constant checking in, but sustained connection
- Less emotional processing help, but continued validation that grief doesn't follow linear paths
- Less practical assistance with daily functioning, but help navigating new challenges (dating after loss, family changes, new relationships)
These changes don't mean you're "better" or "over it." They mean you're integrating loss into your life in ways that allow more breathing room. Healthy support systems adapt to these changes rather than maintaining early-grief intensity indefinitely or disappearing completely.
Giving Back When Ready
Some people eventually feel called to support others who are grieving. This might look like volunteering with grief organizations, participating in support groups, or simply being available to friends experiencing new losses.
There's no obligation to do this work, and there's no timeline for when you "should" be ready. Some people never feel called to formalize their support of other grievers, and that's perfectly fine. But for those who do, giving back can be part of meaning-making and honoring loved ones.
The key is ensuring you're giving from fullness rather than depletion. Grief support given when you're still struggling often leaves everyone depleted. But when you've found some degree of integration and stability, supporting others can be deeply meaningful for everyone involved.
Try This: Create a support maintenance plan. Who are the people you want to stay connected with? How often do you need contact? What specific days do you want acknowledged? Share this information with your support system. Making needs explicit reduces the burden of hoping people will remember or know what you need.

Your Path Forward
Building and maintaining a grief support system is hard work, especially when you're already depleted by loss. But this work matters. Research consistently shows that social support is one of the most significant protective factors in grief (Lobb et al., 2010). The effort you put into identifying, asking for, and receiving support literally changes your grief trajectory.
Here's what we hope you'll remember:
- You deserve support, regardless of how long it's been or how you think you "should" be feeling. Grief looks different for everyone, and your needs are valid even if they don't match what others expect.
- Support systems require multiple people serving different functions. No single person can meet all your grief needs. Building varied support protects everyone from burnout and ensures different aspects of your grief get attention.
- Asking for help is a skill that improves with practice. The discomfort of being vulnerable doesn't mean you're doing it wrong. It means you're being brave enough to let people in during a difficult time.
- Your support needs will change, and that's expected. What helps at three months after loss might be different from what helps at three years. Healthy support systems adapt to these changes rather than remaining static.
- Professional support, peer support, and personal network support each offer something unique. You might benefit from all three, or you might find one or two sources sufficient. There's no single right configuration.
Memorial decisions, including how you maintain physical connection to your loved one, are deeply personal choices best made with support but ultimately decided by you. Whether you choose traditional options or alternatives like solidified remains, what matters is that your choice aligns with how you need to remember and honor your person.
Start with one small step: Identify one person in your life who might be able to provide one type of support you need right now. Make one specific request. Notice what happens. Build from there.
Grief is lonely enough without trying to do it alone. You're allowed to need people. You're allowed to ask for help. You're allowed to build a support system that actually helps rather than trying to make do with what feels inadequate.
This is hard work, and you're doing it. That matters.
Frequently Asked Questions
How do I know if I need grief support?
If you're asking this question, you probably do. Signs include feeling isolated or misunderstood, struggling with daily functioning, having difficulty making decisions, experiencing physical symptoms (sleep problems, appetite changes, fatigue), or feeling overwhelmed by grief intensity. But you don't need to meet a crisis threshold to deserve support. Grief is inherently difficult, and most people benefit from support even when they're functioning adequately.
What if I feel like I'm burdening people by asking for support?
This is one of the most common grief concerns, and research shows it's usually not accurate. People generally want to help; they just don't know how (Breen & O'Connor, 2011). When you make specific requests, you actually make it easier for others to show up meaningfully. Most supporters feel relieved to have clear direction rather than guessing what might help. If specific people show signs of burnout or frustration, that might mean you need to add more people to your support system rather than assuming you're inherently too much.
Is it normal to need support years after a loss?
Absolutely. Grief doesn't follow linear timelines, and the idea that you should be "over it" after a certain period isn't based on how grief actually works. Integration is a lifelong process, and while grief typically becomes less intense and pervasive over time, you'll likely always have moments when you need support. Anniversary reactions, milestone dates, and unexpected triggers can intensify grief even years after loss. Needing support during these times is completely normal.
What if my friends and family don't understand my grief?
This is incredibly painful and unfortunately common. Some possibilities include: (1) They may care deeply but not know how to express it, (2) They might be uncomfortable with grief generally and avoid it, (3) They may have different grief styles that make your expression confusing to them, or (4) They might be dealing with their own unprocessed losses that make your grief triggering. You might try educating them about your specific needs, seeking out grief-specific support groups where understanding is built-in, or supplementing family support with professional counseling. You can love people who can't support your grief well while also recognizing you need to find support elsewhere.
How do I support myself through memorial decisions?
Memorial decisions work best when you give yourself permission to move at your own pace. Consider involving trusted support people in exploring options, but make the final decision based on what feels right for you and your family. Some helpful questions include: How do I want to maintain physical connection to my loved one? What options allow for sharing among family members if that's important? What feels meaningful rather than just traditional? Would I benefit from waiting until I have more clarity? There's no universal right answer. Options like burial, scattering, keeping remains at home, or choosing alternatives like solidified remains all serve different families' needs. The process typically becomes clearer when you have support people helping you think through options without pressure.
Can I change my support system if it's not working?
Yes, and you should. Support systems aren't static. People's capacity changes, your needs evolve, and sometimes initial support sources don't work long-term. You can add new people, reduce contact with unhelpful supporters, join and leave groups, or change how you engage with professional support. Making these changes isn't disloyal or ungrateful. It's recognizing that your healing matters and that you deserve support that actually helps rather than making grief harder.
References
Breen, L. J., & O'Connor, M. (2011). Family and social networks after bereavement: Experiences of support, change and isolation. Journal of Family Therapy, 33(1), 98-120. https://doi.org/10.1111/j.1467-6427.2010.00495.x
Klass, D., Silverman, P. R., & Nickman, S. (1996). Continuing bonds: New understandings of grief. Taylor & Francis. https://doi.org/10.4324/9781315800790
Lobb, E. A., Kristjanson, L. J., Aoun, S. M., Monterosso, L., Halkett, G. K., & Davies, A. (2010). Predictors of complicated grief: A systematic review of empirical studies. Death Studies, 34(8), 673-698. https://doi.org/10.1080/07481187.2010.496686
O'Connor, M. F., Wellisch, D. K., Stanton, A. L., Eisenberger, N. I., Irwin, M. R., & Lieberman, M. D. (2008). Craving love? Enduring grief activates brain's reward center. NeuroImage, 42(2), 969-972. https://doi.org/10.1016/j.neuroimage.2008.04.256
Stroebe, M., & Schut, H. (1999). The dual process model of coping with bereavement: Rationale and description. Death Studies, 23(3), 197-224. https://doi.org/10.1080/074811899201046
American Psychological Association. (2020). Grief: Coping with the loss of your loved one. https://www.apa.org/topics/families/grief
HelpGuide.org. (2024). Coping with grief and loss. https://www.helpguide.org/mental-health/grief/coping-with-grief-and-loss
National Alliance for Grieving Children. (2024). Finding support. https://childrengrieve.org/
National Institute on Aging. (2024). Coping with grief and loss. https://www.nia.nih.gov/health/grief-and-mourning/coping-grief-and-loss
What's Your Grief. (2024). Grief support resources. https://whatsyourgrief.com/